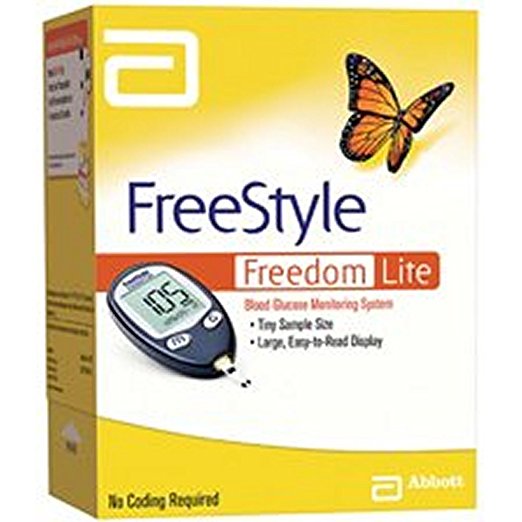
FreeStyle Lite test strips 50 count
FreeStyle Lite test strips 50 count
about the product
- 50 test strips per box
- Tiny sample size – only 0.3 µL
- Patented ZipWik tabs that make application quick and easy
- Up to 60 seconds to re-apply blood means FEWER wasted test strips
- No coding means one less step
How to test your blood sugar
Whether you test several times a day or only once, following a testing routine will help you prevent infection, return true results, and better monitor your blood sugar. Here’s a step-by-step routine you can follow:
- Wash your hands with warm, soapy water. Then dry them well with a clean towel. If you use an alcohol swab, be sure to let the area dry completely before testing.
- Prepare a clean lancet device by inserting a clean needle. This spring-loaded device that holds the needle is what you will use to prick the end of your finger.
- Remove one test strip from your bottle or box of strips. Be sure to close the bottle or box completely to avoid contaminating the other strips with dirt or moisture.
- All modern meters now have you insert the strip into the meter before you collect blood, so you can add the blood sample to the strip when it is in the meter. With some older meters, you put the blood on the strip first, and then put the strip in the meter.
- Stick the side of your fingertip with the lancet. Some blood sugar machines allow for testing from different sites on your body, such as the arm. Read your device’s manual to make sure you’re drawing blood from the correct place.
- Collect a drop of blood on the test strip, making sure you have an adequate amount for a reading. Be careful to let only the blood, not your skin, touch the strip. Residue from food or medication may affect the test’s results.
- Stop the bleeding by holding a clean cotton ball or gauze pad on the end of the finger. Apply pressure on the fingertip until the bleeding has stopped.
Six tips for successful blood sugar monitoring
- Keep your meter and supplies (lancets, alcohol swabs, testing strips, and so on) with you at all times.
- Make sure your testing strips aren’t expired. Out-of-date strips are not guaranteed to return true results. Old strips and inaccurate results may affect your daily log of blood glucose numbers, and your doctor may think there’s a problem when there really isn’t. Also, keep the strips out of sunlight and away from moisture. Keep them at room temperature or cooler, but not freezing.
- With the help of your doctor, establish a routine for how often and when you should test your blood sugar. They may suggest checking it while you’re fasting, before and after meals, or before bedtime. Each person’s situation is different, so it’s important to decide on an arrangement that will work for you. When you have that schedule, make checking your blood part of your daily routine. Build it into your day. Many meters have alarms that you can set to help you to remember to test. When it’s part of the day, you’ll be less likely to forget.
- Don’t assume that your meter is correct. Most meters come with a control solution that allows you to test to see how accurate your meter and strips are. Take your blood glucose meter with you to your next doctor’s appointment. Compare your results with those of their machine to see whether there are any possible discrepancies.
- Create a journal to log your blood sugar each time you test it. Apps are available that can track this information and help you keep a running tally of your average blood sugar. You may also choose to record in a notebook or blood sugar diary the time of day you tested and how long it had been since you had eaten anything. This information will help your doctor track your blood sugar and may become very important when diagnosing what is causing your blood sugar to spike.
- To avoid infection, practice the Centers for Disease Control and Prevention strategies for safe injections. Don’t share your blood sugar monitoring equipment with anyone, dispose of the lancet and strip after each use, and be careful to wait until your finger has stopped bleeding to resume activities.
Read more: Why glucose meter and strip accuracy matters »
PREVENTING SORE FINGERTIPS
Preventing sore fingertips
Frequent and repeated testing can cause sore fingertips. Here are a few suggestions that may help prevent this:
- Don’t reuse a lancet. They can become dull, which may make pricking your fingers painful.
- Be sure to prick the side of your finger, not the pad. Pricking the end of your finger can be more painful.
- Though it may be a tempting way to produce more blood quickly, don’t squeeze your fingertip vigorously. Instead, hang your hand and arm down, allowing blood to pool in your fingertips. You can also help increase blood flow by washing your hands with warm water. If you still have too little blood, you can squeeze your finger, but start at the part closest to your palm, working your way down your finger until you have enough.
- Don’t test on the same finger each time. As part of your routine, establish which finger you’ll use and when so that you never repeat on the same finger during the same day.
- If a finger becomes sore anyway, avoid prolonging the pain by not using it for several days. Use a different finger if possible.
- If you have chronic finger pain as a result of testing, see your doctor about changing glucose monitors. Some monitors can use blood drawn from other parts of the body.
Read more: A patient’s review of the new Dario glucose meter »
THINGS TO WATCH OUT FOR
Things to watch out for
Being asked by your doctor to monitor your glucose levels is an important part of the diagnostic process. Remember that many things can affect blood sugar, including:
- what and when you’ve last eaten
- what time of day you check your blood sugar
- your hormone levels
- infection or illness
- your medication
Be mindful of the “dawn phenomenon,” a surge of hormones that happens around 4:00 a.m. for most people. This can affect glucose levels.
Speak to your doctor about any concerns or questions that you have before beginning a routine of blood sugar monitoring. If your blood glucose result is wildly different each day in spite of consistent testing behavior, there may be something wrong with your monitor or the way that you’re taking the test.
Issues that affect your glucose level
Health conditions such as diabetes and hypoglycemia will obviously have a big impact on your blood sugar levels. Pregnancy can also affect your blood sugar, which sometimes results in gestational diabetes for the duration of the pregnancy.
ABNORMAL GLUCOSE LEVELS
What to do if your glucose levels are abnormal
The American Diabetes Association points out that every person’s recommended blood sugar level is different and is based on several health factors. But, in general, the target range for glucose levels is 80-130 milligrams/deciliter (mg/dl) before eating and less than 180 mg/dl after a meal.
If your glucose levels don’t fall within the normal range, you and your doctor will need to make a plan to determine the reason why. Additional testing for diabetes, hypoglycemia, certain medical conditions, and other endocrine issues may be necessary to identify why your blood sugar is too high or too low. Continue to monitor your blood glucose levels while you wait on test appointments or test results. If you experience any of the following symptoms, then let your doctor know right away:
- dizziness
- sudden onset migraines
- swelling
- loss of feeling in your feet or hands
TAKEAWAY
Takeaway
Monitoring your blood glucose level yourself is fairly straightforward and easy to do. Though the idea of taking a sample of your own blood each day makes some people squeamish, the modern spring-loaded lancet monitors make the process nearly painless. Logging your blood glucose levels can be part of a healthy diabetes maintenance or dietary routine.
Article resources
Email this page
Your full nameYour emailRecipient’s email
SEND EMAIL
Your privacy is important to us
How helpful was it?
This article changed my life!This article was informative.I have a medical question.
How can we improve it?
This article contains incorrect information.This article doesn’t have the information I’m looking for.I have a medical question.
Medically reviewed by Judith Marcin, MDon April 24, 2017 — Written by Kimberly Holland and Kathryn Watson
top stories
COLD & FLU
2018 Flu Season Off to a Strong, Potentially Dangerous StartEXERCISE
Annual Gym Memberships Can Be a Trap. Do This Instead.NUTRITION
19 Foods That Can Fight Sugar CravingsWOMEN'S HEALTH
Why Do So Many Older Women Have Eating Disorders?DIABETES
Why So Many People with Diabetes Stop Taking Metformin